Prostate
- Home >
- Prostate
The two standard prostate cancer screening tests for detection include:
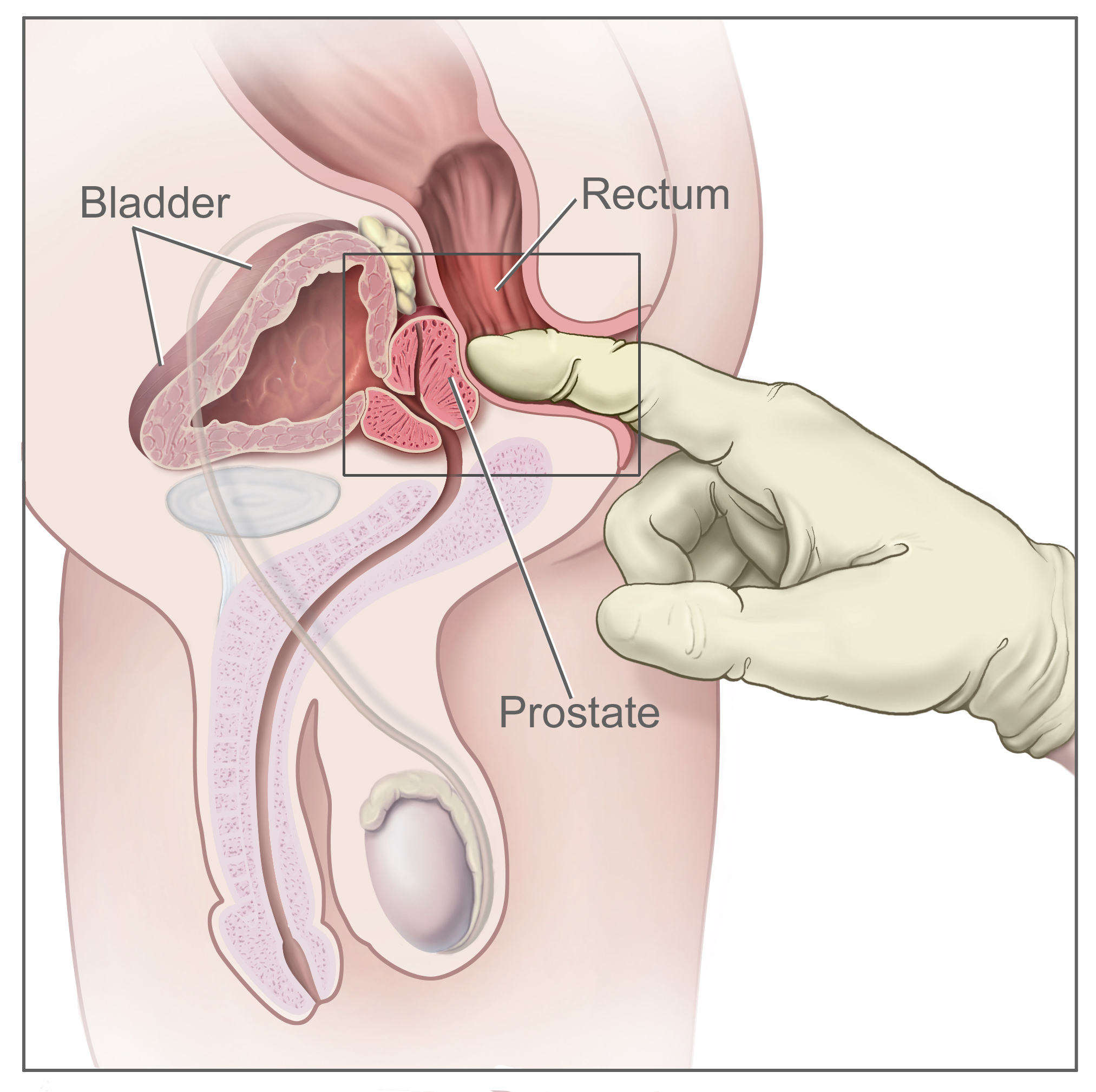
- Digital rectal exam (DRE): - During this test, the doctor inserts a gloved finger into the rectum to feel the prostate for irregularities in size and texture, such as hardness or a nodule (small rounded bump).
- PSA test - This measures the level of prostate-specific antigen (PSA) in the blood. PSA is a protein made by cells in the prostate gland. Your doctor may talk about a normal PSA level. There is not one normal PSA level for everyone. The PSA level naturally gets higher as you get older and varies depending on the size of your prostate.
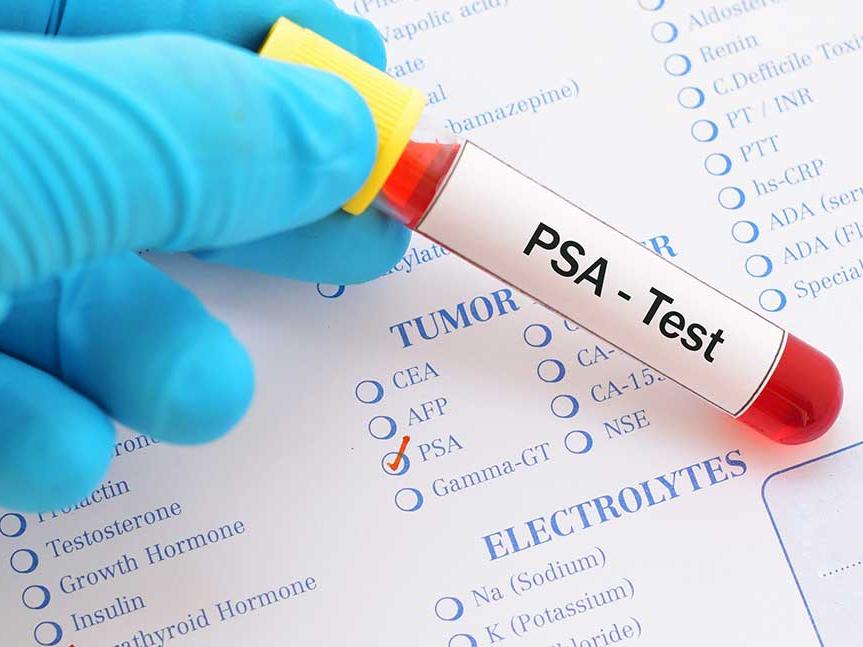
An increased PSA level can indicate a problem with your prostate. This could be:
- An enlarged prostate (BPH) Benign prostate hyperplasia
- Prostatitis (Infection of the prostate)
- Prostate cancer
Other factors that may increase PSA levels may include:
- Recent ejaculation
- Vigorous exercise such as riding a bicycle
- Certain medications such as hormone therapy i.e. Testosterone
- Urinary tract infections
Your doctor will tell you what they think the normal level of PSA should be for you. They generally use the following table as a guide:
| Age Range | PSA Level |
|---|---|
| 40-49 | 0-2.5 |
| 50-59 | 0-4.0 |
| 60-69 | 0-4.5 |
| 70-79 | 0-5.5 |
Most men without prostate cancer have PSA levels under 4 ng/mL of blood.
When prostate cancer develops, the PSA level often goes above 4. Still, a level below 4 is not a guarantee that a man doesn’t have cancer. About 15% of men with a PSA below 4 will have prostate cancer if a biopsy is done.
Men with a PSA level between 4 and 10 (often called the “borderline range”) have about a 1 in 4 chance of having prostate cancer.
If the PSA is more than 10, the chance of having prostate cancer is over 50%.
Other tests may include:
A transrectal ultrasound (TRUS) provides images of a man’s prostate gland and surrounding tissue. The exam requires insertion of an ultrasound probe into the rectum of the patient. It is used to estimate the size of the prostate gland, helping doctors get a better idea of PSA density, which helps distinguish benign prostatic hyperplasia (BPH) from prostate cancer. Measurements acquired are used to plan treatment.
DIAGNOSIS
Your doctor will evaluate the results of the screening tests and may recommend a repeat test or a biopsy. This biopsy involves using a fine hollow needle to take small samples of prostate tissue that are analysed under a microscope to determine the presence of cancer cells. To ensure the best samples are taken, a transrectal ultrasound (TRUS) is used.
A TRUS guided biopsy involves placing a needle through the wall of the rectum (transrectal) or less commonly practiced, through the perineum (transperineal), the area between the scrotum and the rectum, to obtain prostate tissue.
It is essential for prognosis and decision making. The table below describes the different Gleason scores and grade groups that can be given after a prostate biopsy. This is just a guide.
| Group | Gleason Score | Description | Risk Level |
|---|---|---|---|
| 1 | 6 (3+3) | All of the cancer cells found in the biopsy look likely to grow slowly. | Low risk |
| 2 | 7 (3+4) | Most of the cancer cells found in the biopsy look likely to grow very slowly. There are some cancer cells that look likely to grow at a moderately quick rate | Medium |
| 3 | 7 (4+3) | Most of the cancer cells found in the biopsy look likely to grow at a moderately quick rate. | Medium |
| 4 | 8 (3+5) | Most of the cancer cells found in the biopsy look likely to grow very slowly. There are some cancer cells that look likely to grow quickly. | High |
| 8 (4+4) | Most of the cancer cells found in the biopsy look likely to grow at a moderately quick rate. | High | |
| 8 (5+3) | Most of the cancer cells found in the biopsy look likely to grow quickly. There are some cancer cells that look likely to very slowly. | High | |
| 5 | 9 (4+5) | Most of the cancer cells found in the biopsy look likely to grow at a moderately quick rate. There are some cancer cells that look likely to grow quickly. | High |
| 10 (5+5) | All the cancer cells found in the biopsy that look likely to grow quickly. | High |
Staging of Prostate Cancer
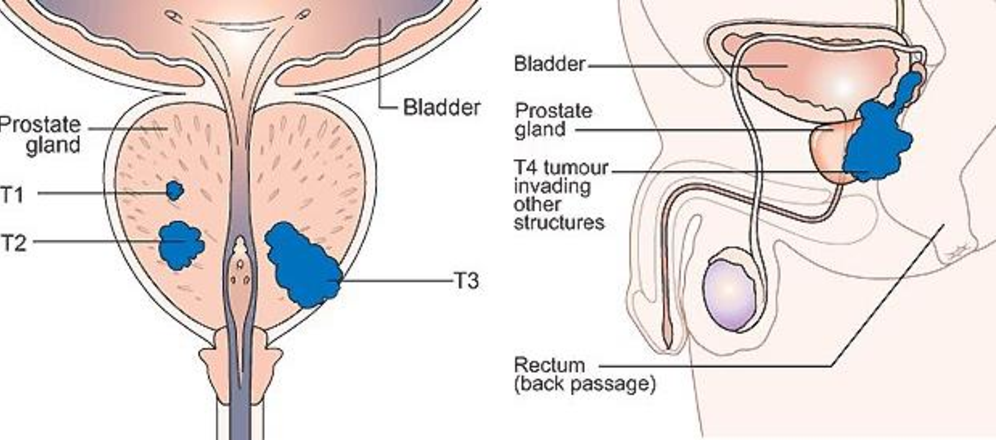
Staging of prostate cancer determines if it has spread beyond the prostate. This is usually recorded using the TNM (Tumour-Nodes-Metastases) system.
The T stage shows how far the cancer has spread in and around the prostate.
The N stage shows whether the cancer has spread to the lymph nodes.
The M stage shows whether the cancer has spread (metastasised) to other parts of the body
The doctor may recommend having a CT, bone scan or Multiparametric MRI to determine if the cancer cells have spread outside the prostate capsule. The results of both the scan and the biopsy will assist in determining if the stage of cancer is localised, locally advanced or advanced. This will allow you and your doctor to decide which treatment options may be best for you.
Localised:
- T1 & T2: The tumour is located in the prostate only.
- T3: The tumour has breached the prostate capsule on 1 or more sides.
- T3b: The tumour has begun to grow in the seminal vesicles.
- T4: The tumour has grown into other neighbouring structures, like the bladder, the rectum, the pelvic wall or lymph nodes.
Locally Advanced
Prostate cancer has spread to the area just outside the prostate capsule. The spread of cancer is measured in two ways: by lymph node involvement, and by its appearance in other organs or parts of the body, or metastasis. Lymph node staging, or N-staging, determines whether the cancer is present in nearby lymph nodes. Lymph nodes are tiny organs that are part of the immune system.
- NX: The regional lymph nodes cannot be evaluated.
- N0: The cancer has not spread to lymph nodes in the immediate area.
- N1: The cancer has spread to lymph nodes in the pelvic region.
Advanced
The "M" in the TNM system indicates whether the prostate cancer has spread to other parts of the body, such as the lungs or the bones. This is called distant metastasis.
- MX: Metastasis cannot be evaluated.
- M0: The cancer has not metastasized beyond the immediate prostate region.
- M1: The cancer has metastasized to other parts of the body outside the pelvis.
- M1a: The cancer has spread to lymph nodes away from the groin area.
- M1b: The cancer has spread to the bones
- M1c: The cancer has spread to another part of the body, with or without spread to the bones.
The combination of your full staging results, including your grade and your T, N, and M stages, paints a more complete picture of how the cancer is progressing. This enables your doctor to determine your risk and which treatments have the best chance of eradicating your cancer.
Symptoms of Prostate Cancer
Many men with localised or early stage prostate cancer have no noticeable symptoms as the cancer is confined to the capsule of the prostate gland. Often the first sign of the disease is an abnormal finding on a routine check-up by a doctor. Some men, may experience changes in urinary and sexual function that may indicate the presence of prostate cancer. Symptoms may be similar to that of an enlarged prostate or benign prostatic hyperplasia (BPH). Common symptoms of BPH may include:
- Frequent or urgent need to urinate
- Difficulty urinating or waking more frequently during the night to urinate
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Inability to completely empty the bladder
In locally advanced prostate cancer, abnormal cancer cells have broken through the capsule (covering) of the prostate gland. It may have spread into the:
- tissue around the prostate
- the tubes that carry semen (seminal vesicles)
- body organs nearby such as the back passage (rectum) or neck of the bladder
- lymph nodes close to the prostate gland
Symptoms of locally advanced prostate cancer may include:
- Difficulty urinating
- Pain in the lower back, hips or upper thighs
- Problems getting or keeping an erection
- Blood in urine or semen
- Unexplained weight loss
- Swelling of legs (lymphoedema) caused by blockage of lymph glands.
Abnormal prostate cancer cells may invade the blood stream or lymphatic system spreading to other parts of the body. This is called metastatic prostate cancer and the most common areas likely to be affected are the adrenal glands, bones, liver and lungs.
Symptoms of metastatic prostate cancer may include:
- Fatigue
- Bone pain
- Weak bones, increasing your risk for fractures
- Spinal cord compression
- High blood calcium levels
- Stiffness or pain in the hip, thighs or back
You should consult with your doctor if you experience any of the symptoms above so that you can be sure to get a proper diagnosis and treatment if needed.
Prostate cancer is the most common form of cancer found in men in Trinidad and Tobago and accounts for 39% of all cancer related mortality among men. The Elizabeth Quamina National Cancer Registry documented an incidence rate of 60.4/100,000 for the period 1995-2002.
Normal cells reproduce themselves by dividing and replacing worn-out and injured cells. Cancer is characterized by the uncontrolled growth of abnormal cells which sometimes grow into a tumour mass and prostate cancer is no different. Doctors can describe prostate cancer as localised, locally advanced and advanced.
As with many forms of cancers, early detection provides the greatest chance of a cure. For this reason, it is important for all men over the age of 50 be screened annually. However, men of African descent or those who have a family history of prostate cancer are at a higher risk. For this group screening should begin at 40 years of age.
Risk Factors
The exact cause of prostate cancer is unknown but research has shown that men with certain risk factors are more likely than others to develop prostate cancer. Having a risk factor, does not mean that you will get prostate cancer but rather you may be more at risk of developing the disease. The three main risk factors of developing prostate cancer are as follows:
Age
The chance of getting prostate cancer increases with age. Men over the age of 45 have a higher risk than younger men.
Family History
Prostate cancer risk is approximately 2 to 3 times greater for men whose fathers or brothers have had the disease. Prostate cancer risk also appears to be slightly higher for men whose mothers or sisters have had breast cancer.
Ethnicity
Prostate cancer is more common in men of African or mixed African ethnicity. The cause is unknown but may be linked to genes. We know that Afro-Trinbagonians are at greater risk, than Indo-Trinbagonians of developing prostate cancer.
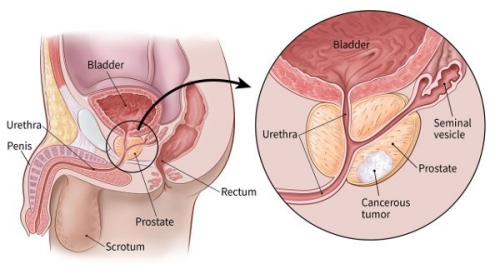
The prostate gland is found only in men. It is a key part of the male reproductive system that produces the fluid which transports sperm during ejaculation. The prostate gland is approximately the size and shape of a walnut and is located in front of the rectum and below the bladder. If it is enlarged, can in fact push against it. Additionally, the tube that carries the urine out of the bladder, called the urethra, always passes directly through the prostate.
It is because of this intimate relationship between prostate, bladder and urethra that abnormalities of the prostate often result in urinary problems.
The prostate is also located directly in front of the rectum. In fact, the only way for your doctor to feel the surface of the prostate, so as to properly examine it, is through the rectum.

It has been found that the prostate is a very common location for cancer to begin. Regular examination of the prostate is therefore vital to male health.
